A peak flow meter is a device that helps you know how well controlled your asthma is and how well your lungs are working at any given point in time. For people with asthma, it is a simple but important tool to help with daily asthma management.
The readings from the meter will help you and your pulmonologist:
- Determine the severity of your disease.
- Evaluate the effectiveness of your current medications.
- Determine when to add or stop certain medicines.
- Recognize an asthma attack before signs or symptoms appear.
- Decide when to seek emergency care.
Risks and Complications of using Peak Flow Meter
There is no serious risk associated with peak flow meter. When you are using the peak flow meter, breathing too quickly may cause dizziness. At an extreme, this could cause you to pass out. Take your time so you do not get dizzy or light-headed.
How to find your personal best
Your “personal best” is the highest peak flow rate you can reach when you feel good and have no asthma symptoms. This can be used as your baseline against which you can compare your peak flow meter readings. Because everyone’s asthma is different, your personal best will be unique to you.
Your pulmonologist will help you figure out your personal best. Typically, you will take readings once or twice a day for 2 weeks when you are not having symptoms. The highest reading during the trial period is your personal best. Because your lung function can change over time, your personal best should be remeasured each year.
How to use your Peak Flow Meter
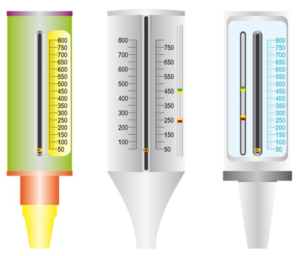
- Move the upper marker to the number that is your personal best
- Move the lower marker to the bottom of the numbered scale.
- Connect the mouthpiece to the peak flow meter.
- Stand up.
- Take a deep breath. Make sure you fill your lungs completely.
- Place your lips tightly around the mouthpiece. Blow as hard and as fast as you can with a single breath (forced exhalation), as if you are blowing out candles. If your lips are not placed tightly around the mouthpiece of the peak flow meter, you will get incorrect low readings.
- At the end of your forced exhale, check to see what number the lower marker landed on. This is your peak flow rate.
- Move the lower marker back to the bottom of the numbered scale.
- Repeat these steps 2 more times. Record the highest reading of the 3 tries in your asthma diary. Do not calculate the average for your 3 tries, just record the highest.
Always write down the results in your asthma diary. After using your peak flow meter, rest and breathe slowly and easily. Keep a record of your progress. Your health care provider can provide you with a simple table to help with this. For the most accurate readings, it is important to keep your peak flow meter clean. Follow the manufacturer’s instructions on how to take care of your peak flow meter.
Your pulmonologist will give you instructions on when to do regular monitoring. You may also need to check your peak flow when:
- Coughing, wheezing, or other asthma symptoms wake you up at night.
- Your asthma symptoms worsen during the day.
- Your breathing is made worse because of a cold, flu, or other respiratory illness.
- You need to use your quick-relief, “rescue medicine.” It is best to check your peak flow rate before you use rescue medicine, and then 20-30 minutes afterward. This will help determine whether you need to repeat taking the rescue medicine.
How to use your results
You and your pulmonologist can use color-coded zones on the meter to see how your peak flow rate compares to your personal best. The color code for each zone reflects progressively more severe symptoms:
Green Zone = Stable
- Peak flow rate between 80% and 100% of your personal best. Your asthma is under good control when your peak flow rate is in the green zone.
- When you are in the green zone, you are not likely to be experiencing any asthma symptoms.
- Only take your regular, preventive medicine. Your rescue medicine is not required.
Yellow Zone = Caution
- Peak flow rate between 50% and 80% of your personal best. Your asthma is getting worse and could be improved.
- You may have begun coughing, wheezing, or feeling chest tightness. Sometimes peak flow rates dip down into the yellow zone before asthma symptoms appear.
- Consider increasing or changing your asthma medicine. This may include using your rescue medicine. If you have an asthma action plan, follow each step listed for the yellow zone, including medicine changes.
Red Zone = Danger
- Peak flow rate below 50% of your personal best. This may mean you are having, or are at risk of having, a medical emergency.
- Your coughing, wheezing, or shortness of breath may have become severe. Do not wait to use your rescue medicine. Stop whatever you are doing and use your rescue inhaler, nebulizer, or other medicines to open your airways.
- If you have an asthma action plan, follow each step listed for the red zone, including medicine changes and when to seek emergency medical care.
- If your flow readings fall too far below your personal best into the yellow or red zone, you will need to take action to prevent or minimize an asthma attack.
Seek medical care if
- You are in the yellow zone. If you have an asthma action plan, follow all of the steps listed under the yellow zone section of the plan. Let your pulmonologist provider know that you are in the yellow zone.
- You are in the red zone. If you have an asthma action plan, follow all of the steps listed under the red zone section of the plan while you are seeking immediate medical care.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.

